As the medical community continues to uncover the long-term effects of COVID-19, one condition has been showing up with increasing frequency: Postural Orthostatic Tachycardia Syndrome (POTS). Patients recovering from even mild COVID-19 infections are reporting symptoms that look strikingly like autonomic dysfunction — especially elevated heart rates, fatigue, dizziness, and brain fog upon standing.

But is there a real link between COVID-19 and POTS? Or are we seeing a spike in POTS diagnoses simply due to increased awareness?
In this article, we’ll explore what we know, what’s still unclear, and what patients in Maryland and beyond should understand when seeking diagnosis and treatment.
What Is POTS?
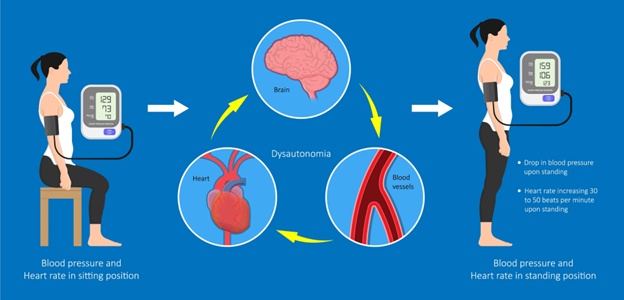
POTS (Postural Orthostatic Tachycardia Syndrome) is a form of dysautonomia, meaning it involves dysfunction of the autonomic nervous system—the part of your body that controls automatic processes like heart rate, digestion, and blood pressure.
In people with POTS, standing up causes the heart rate to spike dramatically—by 30 beats per minute (bpm) or more within 10 minutes of standing (or 40 bpm for children and adolescents), without a corresponding drop in blood pressure.
Common POTS Symptoms:
- Rapid heartbeat (tachycardia)
- Lightheadedness or dizziness
- Fatigue and exercise intolerance
- Brain fog
- Nausea or GI discomfort
- Cold hands and feet
- Shortness of breath
- Sleep disturbances
POTS is not life-threatening, but it can be severely life-altering—making simple tasks like standing in line or walking up stairs exhausting.
COVID-19’s Impact on the Autonomic Nervous System

COVID-19 primarily targets the respiratory system, but its impact reaches much further. In some individuals, the virus appears to cause lasting damage to the autonomic nervous system, particularly in those who go on to develop Long COVID.
Possible Mechanisms:
- Autoimmunity: COVID-19 may trigger the body to produce autoantibodies that mistakenly attack the autonomic nervous system.
- Viral persistence: The virus may linger in nervous system tissues.
- Inflammation: Systemic inflammation may disrupt nerve signaling and vascular tone.
- Vascular damage: COVID-related inflammation could lead to venous pooling, a key contributor to POTS symptoms.
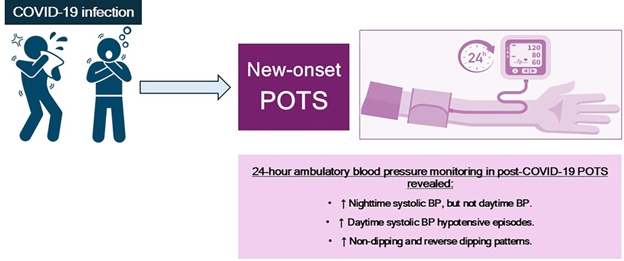
These factors are still being investigated, but early studies suggest a strong association between COVID-19 and new-onset POTS—particularly within 6 to 8 months post-infection.
Who Is Most at Risk?
While anyone recovering from COVID-19 could develop POTS, data shows that the condition tends to affect:
- Females (around 80–90% of cases)
- People aged 15–45
- Individuals with a history of autoimmune disorders or migraines
- Patients with Long COVID symptoms lasting more than 3 months
In our POTS clinic in Maryland, we’ve seen a notable increase in post-COVID patients fitting this profile.
COVID-19 Vaccines and POTS: What We Know
Some patients have reported developing POTS symptoms following COVID-19 vaccination, particularly after mRNA vaccines. However, large-scale studies suggest this is rare, and far less likely than developing POTS after a COVID-19 infection.
One study of nearly 285,000 people found that the risk of POTS was five times higher in unvaccinated individuals with COVID-19 than in vaccinated individuals.
Bottom Line:
The benefits of vaccination outweigh the risks. Vaccines remain one of the best tools for preventing both acute COVID-19 and its long-term complications like POTS.
Diagnosing POTS Post-COVID
POTS is frequently misdiagnosed or dismissed as anxiety, especially in younger women. Diagnosis requires both clinical suspicion and objective testing.
Key Diagnostic Tools:
- Active Stand Test or Tilt Table Test: Measures heart rate and blood pressure changes with posture.
- 24-hour Holter Monitor: Tracks heart rhythms throughout daily activities.
- Bloodwork: Evaluates thyroid function, B12 levels, autoimmune markers, and plasma volume.
- Autonomic Testing: When available, this offers a full picture of autonomic function.
At our POTS clinic in Maryland, we often see patients who’ve bounced between multiple providers before receiving a correct diagnosis.
If you’re searching for a POTS doctor accepting new patients in MD, make sure they understand how COVID-19 and POTS interact.
POTS Treatment After COVID-19
There is no single cure for POTS, but with the right treatment approach, many patients experience significant improvement or even remission of symptoms.
Lifestyle First:
- Hydration & Salt: 2–3 liters of water and up to 10g of salt daily (under supervision)
- Compression garments: Especially abdominal and thigh-high stockings
- Elevated sleeping position: Head of bed raised by 4–6 inches
- Small, frequent meals: Avoid heavy or carbohydrate-rich meals
- Temperature control: Avoid hot showers and overheating
Exercise Approach:
Exercise is both crucial and complicated for POTS patients. The goal is recumbent and gradual reconditioning.
Better tolerated options:
- Recumbent cycling
- Swimming
- Rowing machine
Always begin under guidance, ideally with a POTS-informed occupational medicine or physical therapy team.
Medications:
If lifestyle changes don’t bring relief, medications may help:
- Beta-blockers (to control heart rate)
- Fludrocortisone (to retain salt and water)
- Midodrine (to raise blood pressure)
- Ivabradine (for heart rate modulation, sometimes used off-label)
Each patient’s treatment must be individualized, which is why working with a POTS specialist MD is critical.
Why Finding a POTS Doctor in Maryland Matters
POTS is a complex condition often misunderstood by general practitioners. It requires:
- Detailed history-taking
- Pattern recognition of multi-system symptoms
- Coordinated care across cardiology, neurology, and sometimes gastroenterology
A POTS doctor in Maryland who understands the nuances of post-COVID autonomic dysfunction can:
- Prevent misdiagnosis
- Speed up access to proper treatment
- Coordinate follow-ups across specialties
- Support patients emotionally as well as physically
When to Seek Help
If you or someone you know is experiencing:
- Rapid heart rate upon standing
- Dizziness, lightheadedness, or fainting
- Brain fog or fatigue after COVID-19
- Difficulty resuming daily tasks or work
…it’s time to talk to a POTS doctor in MD with post-COVID experience.
Don’t wait until symptoms become overwhelming. Early recognition and intervention can significantly improve quality of life.
Conclusion
The link between COVID-19 and POTS is real — though the full picture is still unfolding. As research continues, what’s clear is this: post-COVID POTS is not in your head. It’s a physiological condition with real, measurable changes in your body.
Whether you’re newly symptomatic or have been struggling for months, support and answers are available.
At Diekman Dysautonomia, we’re not just specialists — we understand what it’s like to live with this condition. Our clinic in Maryland is committed to providing expert care, rooted in both science and empathy.
Looking for a POTS specialist in Maryland who listens and gets it?

