We all feel tired sometimes. But if you’ve ever experienced a level of exhaustion so severe that it disrupts your ability to function — even after a full night’s sleep — it may be more than just stress, overwork, or a poor night’s rest. You might be living with a condition known as POTS, short for Postural Orthostatic Tachycardia Syndrome.

While it’s estimated to affect up to three million Americans, POTS remains one of the most commonly misdiagnosed and least understood conditions — especially when fatigue is the primary symptom. Many patients spend years searching for answers before finding a doctor who recognizes what’s really going on.
In this article, we’ll explore why POTS is often the hidden cause behind extreme fatigue, what other symptoms to watch for, and how patients in Maryland and elsewhere can find support and effective treatment.
What Is POTS?
POTS is a form of dysautonomia, which means it affects the autonomic nervous system — the part of your body that regulates automatic functions like heart rate, blood pressure, digestion, and temperature control.
In someone with POTS, blood tends to pool in the lower body when standing, causing the heart to beat rapidly (30+ beats per minute above resting) in an attempt to circulate blood to the brain. This sudden rise in heart rate, without a significant drop in blood pressure, is a hallmark of the condition.
The result? Dizziness, rapid heartbeat, brain fog, and, for many, debilitating fatigue.
Fatigue: The Symptom That Disrupts Lives
Many people with POTS describe the fatigue as unlike anything they’ve ever experienced. It’s not just tiredness. It’s the feeling of having absolutely no energy left — like the body is running on fumes.
Patients Often Report:
- Waking up exhausted, even after 8–10 hours of sleep
- Sudden energy crashes in the middle of the day
- Inability to complete routine tasks like grocery shopping or showering
- Brain fog so intense it feels impossible to focus or think clearly
For some, this fatigue can come and go unpredictably, lasting hours or even days. For others, it’s a constant presence that shapes their entire life.
It’s no surprise that POTS-related fatigue is often mistaken for chronic fatigue syndrome, depression, or anxiety — and unfortunately, many patients are told the problem is “in their head.”
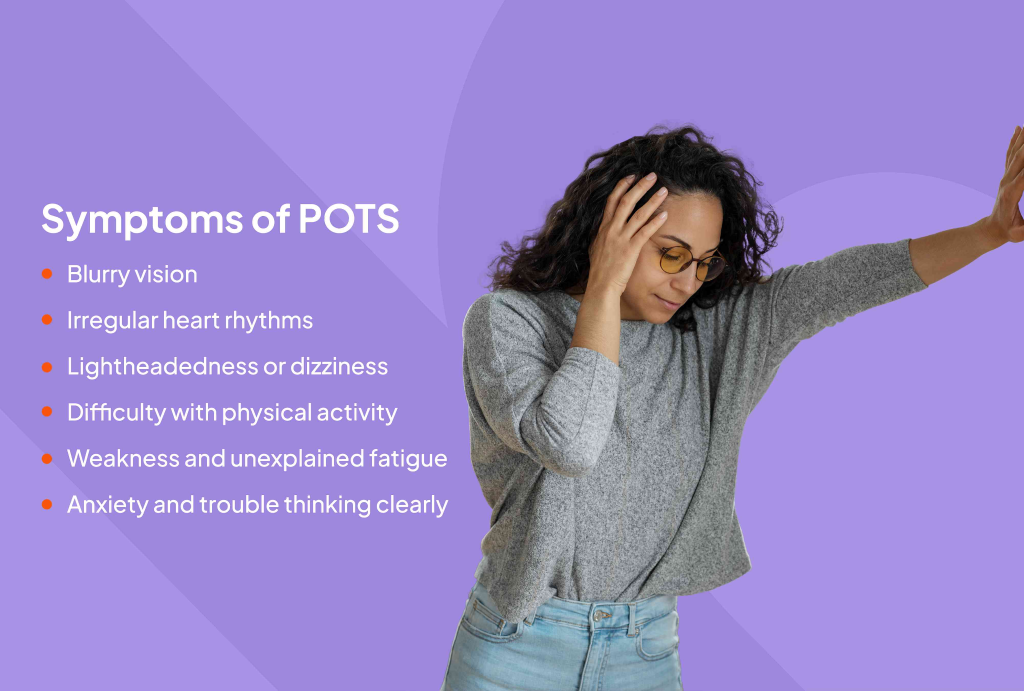
Other Signs of POTS to Watch For
Fatigue is just one piece of the puzzle. POTS affects multiple systems in the body. Many people also experience:
- Dizziness or lightheadedness, especially when standing
- Rapid heartbeat (tachycardia) or heart palpitations
- Fainting or near-fainting episodes
- Brain fog, memory issues, difficulty concentrating
- Nausea, bloating, or GI discomfort
- Temperature regulation issues (sweating too much or too little)
- Shakiness or muscle weakness
- Excessive fatigue after minimal exertion (post-exertional malaise)
The variability and complexity of symptoms is part of why POTS is so frequently misdiagnosed — and why patients often go years without answers.
Who Gets POTS?
POTS can affect anyone, but certain patterns are well-documented:
- 80–90% of patients are women
- Onset is most common between the ages of 15 and 45
- There’s often a family history of autoimmune conditions
- People with Ehlers-Danlos Syndrome (EDS) are at increased risk
- POTS can be triggered by viral infections, physical trauma, or pregnancy
- In many cases, symptoms appear or worsen after COVID-19, as part of Long COVID
In fact, post-COVID POTS is now one of the most common reasons patients seek out a POTS doctor in Maryland and across the country.
Why Is POTS So Fatiguing?
The precise mechanism behind POTS-related fatigue is still being researched, but several factors contribute:
- Autonomic Dysfunction: When the nervous system isn’t regulating heart rate and blood pressure properly, the body must work harder to maintain basic function, which burns energy quickly.
- Poor Blood Flow to the Brain: Reduced blood flow, especially upon standing, can leave patients feeling lightheaded, foggy, and mentally drained.
- Sleep Disruption: Many people with POTS struggle with insomnia or unrefreshing sleep, which compounds fatigue.
- Deconditioning: Fatigue leads to inactivity, which can further weaken the cardiovascular system — creating a cycle that’s hard to break.
- Coexisting Conditions: POTS often overlaps with other disorders like Mast Cell Activation Syndrome (MCAS), Ehlers-Danlos, or autoimmune diseases, all of which can contribute to low energy.
Getting a Diagnosis
Diagnosing POTS starts with listening to the patient’s story. The gold standard test is the tilt table test, where your heart rate and blood pressure are monitored as you’re slowly moved from lying to standing.
Other diagnostic tools may include:
- Active Stand Test
- Holter monitor
- Blood volume testing
- Bloodwork to rule out thyroid issues, anemia, or autoimmune disorders
Because POTS symptoms often mimic other conditions, it’s important to work with a provider who understands the subtleties of postural orthostatic tachycardic syndrome.
If you’re in Maryland and looking for clarity, consider seeing a POTS specialist MD or visiting a POTS clinic in Maryland that’s equipped to handle complex, multi-system conditions.
Treatment and Management
While there is no “cure” for POTS, there are many effective strategies to manage symptoms — especially fatigue.
Lifestyle-Based Treatments
- Increase fluids and salt to expand blood volume
- Wear compression garments, especially thigh-high or abdominal
- Raise the head of the bed by 4–6 inches to prevent blood pooling
- Avoid triggers like heat, large meals, or standing still for long periods
- Break up activity into short bursts with rest in between
Exercise as Treatment
Exercise is often recommended — but it must be tailored carefully. Patients often start with recumbent exercises like:
- Stationary biking
- Rowing
- Swimming
Gradually, endurance and upright tolerance can improve. But it’s crucial to work with a provider who understands POTS treatment and doesn’t push “push through it” mentalities.
Medications (if needed)
If lifestyle changes aren’t enough, medications may help:
- Beta-blockers for heart rate control
- Fludrocortisone to retain salt and fluid
- Midodrine to raise blood pressure
- Ivabradine, used off-label in some cases
The key is individualized care, based on symptom profile and tolerance. That’s why finding a POTS doctor accepting new patients in MD can make a significant difference in outcomes.
Why Early Diagnosis Matters
Living undiagnosed with POTS can be devastating — physically, emotionally, and financially. Many patients are misdiagnosed with anxiety, depression, or even hypochondria, which delays treatment and erodes trust in the medical system.
But POTS is real. And for many patients, simply hearing a name for what they’ve been experiencing is life-changing.
If you or someone you love is dealing with extreme, unexplained fatigue, accompanied by any of the symptoms mentioned above, don’t settle for “it’s just stress.”
Final Thoughts
POTS is a real, life-disrupting condition — and fatigue is one of its most common, yet overlooked, symptoms.
If you’re in Maryland and searching for a POTS doctor, know that help is available. With the right treatment plan, many patients experience significant improvements in both energy levels and overall quality of life.
Need Help?
At Diekman Dysautonomia, we specialize in diagnosing and treating postural orthostatic tachycardic syndrome in MD. We understand how exhausting this journey can be — because we’ve walked it too.

